Silica Clotting Time [SCT]
Introduction
The Silica clotting time [SCT] is essentially an Activated Partial Thromboplastin Time [APTT] test in which Silica replaces Kaolin.
Principles
Colloidal silica suspension is mixed with citrated platelet poor plasma [PPP] and calcium is then added to initiate coagulation via activation of Factor XII. The SCT test contains a low dose of phospholipid which makes is very sensitive as a screening test for a Lupus Anticoagulant [LA.]
In the original test [Ref 2] the greatest sensitivity of the SCT to a LA was not seen when PL was completely absent but at a low PL concentration. This is probably because the SCT without PL is highly variable within each patient group but having a low concentration of PL in the test standardises and maximises its sensitivity. A confirmatory test for a LA can be achieved using the SCT by employing a high PL concentration to neutralise the LA and so demonstrate the PL-dependence of the antibody.
Method
The method is an APTT test using Silica as the activator. Colloidal silica suspension is mixed with platelet poor plasma then calcium is added to initiate coagulation.
| Reagent | Explanation |
|---|---|
| Platelet poor plasma - citrated | A source of coagulation factors, particularly thrombin and fibrinogen. |
| Colloidal Silica suspension | Activator of the intrinsic pathway |
| Phospholipid [PL] | Low and High concentrations of PL are used. A low concentration of PL is used for the SCT as a screening test and a high concentration when it is used as a confirmatory test |
| Calcium | To initiate coagulation |
Heparin will interfere with the test but some commercial kits contain a heparin neutralisation agent e.g. polybrene.
Interpretation
In the context of a prolonged SCT, the possibilities are:
1. Anticoagulant present
2. Factor deficiency
3. Lupus anticoagulant present
It is important, therefore, to exclude anticoagulants or a factor deficiency before requesting LA screening.
Correction Tests
Correction tests are undertaken to establish whether a prolonged SCT at low PL concentration corrects with a high PL concentration, thereby establishing the PL-dependence of the antibody.
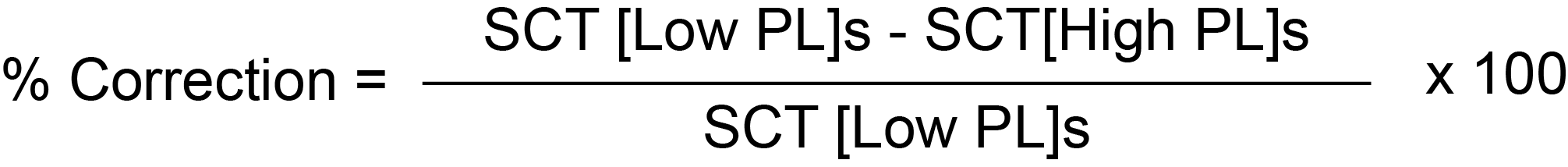
1. Originally [ Ref 2] - the percentage [%] correction was calculated from the equation:
2. In commercial versions of the test:
a. The SCT ratio for the screening test [low PL concentration] is derived from:
Patient Screen SCT [s]/Mean of SCT Screen Reference Range [s]
b. The SCT ratio for the confirmatory test [high PL concentration] is derived from:
Patient Confirm SCT [s]/Mean of SCT Confirm Reference Range [s]
c. The normalised ratio is derived from:
Screen ratio/Confirm ratio
A normalised SCT ratio >1.16 [>1.24 on some machines] indicates the presence of a Lupus Anticoagulant. A ratio < 1.16 [>1.24 on some machines] suggests a factor deficiency.
Look at the following example:
| Sample | SCT Clotting Time [s] | Ratios |
|---|---|---|
| Patient Plasma | 210.3 s | [Patient Plasma]/[Reference Plasma] = 3.22 |
| Reference Control [Normal] Plasma | 65.2 s | |
| Patient Plasma + Phospholipid | 62.2 s | [Patient Plasma + Phospholipid]/Reference Control [Normal] Plasma + Phospholipid] = 1.91 |
| Reference Control [Normal] Plasma + Phospholipid | 32.5 s | |
| Normalised SCT ratio = 3.22/1.91 = 1.68 | ||
From the data above, the normalised SCT ratio is 1.68 and consistent with the presence of a Lupus Anticoagulant.
The Percentage correction is: [3.22 - 1.91/3.22] x 100 = 40.7%.
Reference Ranges
The normalised SCT ratio reference range depends on the machine being used for the test but in general a ratio >1.16 [>1.24 on some machines] indicates the presence of a Lupus Anticoagulant. A ratio < 1.16 [<1.24 on some machines] suggests a factor deficiency.
Interpretation
Commercial versions of this test are relatively insensitive to heparin (up to 0.4 U/ml) because of the presence of polybrene.
The test is also insensitive to oral Anticoagulants and gives a normal result in patients with liver disease and abnormal clotting. The test is less effective at distinguishing between a LA and an anti-FVIII antibody. When a LA is present the SCT confirmatory test is prolonged beyond the SCT screening test i.e. the phospholipid dependant nature of the antibody has been demonstrated.
What Test Next
In individuals in whom a LA is identified, the test should be repeated in 12 weeks. It should also be remembered that not all tests including the SCT will identify all LAs and therefore, if the index of suspicion that a specific patient has a LA then other tests such as the dRVVT should be undertaken.
Finally - the causes of a LA should be screened for e.g. check ANA, drugs, viral serology etc.
