Introduction
VWF binds to collagen via 2 sites - the A3 domain which contains the main site for binding to collagen types I and III [found in the perivascular connective tissue] and a second site in the A1 domain binds which binds non-fibrillar collagen type VI found within the sub-endothelial matrix.
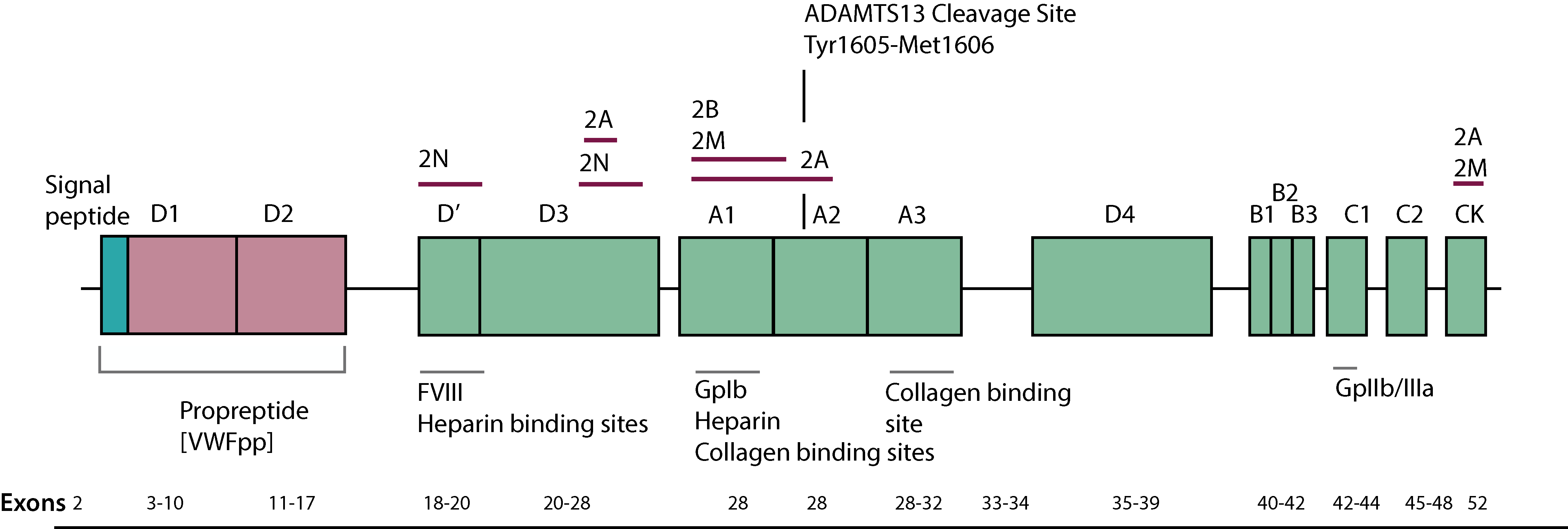
The collagen binding assay [VWF:CB] measures the binding of VWF to collagen and preferentially the High Molecular Weight [HMW] multimers of VWF and is therefore sensitive to VWD variants characterised by the absence of the larger VWF multimers.
The VWF:CB assay stems from concerns over limitations in the sensitivity, reproducibility and inter-laboratory variability of the agglutination-based Von Willebrand Factor Ristocetin cofactor [VWF:RCo] assay. The VWF:CB assay has been shown to be of value in the identification of VWD Type 1, Type 2A and Type 2B VWD.
Principles & Method
VWF:CB activity is measured using Type III or Type I collagen isolated from human placenta. ELISA plates are coated with collagen, patient and control plasma samples are diluted in buffer, aliquots are applied to the ELISA plate, incubated and then washed. A standard curve is constructed from a pool of normal plasma donors. Collagen-bound VWF is detected using a horseradish peroxidase (HRP)–conjugated rabbit anti–human VWF antibody and the change in optical density is proportional to the amount of the VWF bound to the collagen.
Interpretation
The VWF:CB assay has been shown to be of value in the identification of Type 1, Type 2A, Type 2B and Type 3 VWD in which there is a loss of high molecular weight multimers.
| VWD Subtype | Interpretation | Assay Results |
|---|---|---|
| Type 1 | Type 1 VWD, the VWF:CB activity will vary reflecting the degree of loss of High Molecular Weight [HMW] multimers. | ↓ VWF:CB and ↓ VWF:RCo. The VWF:CB assay may be more useful in the diagnosis of Type 1 VWD due to the tighter CV of the assay. |
| Type 2A | In Type 2A VWD there is decreased synthesis [Type Type 2A1 VWD] or increased proteolysis of VWF[Type 2A2 VWD] leading to the loss of HMW multimers. | ↓ VWF:CB and ↓ VWF:RCo |
| Type 2B | in Type 2B VWD increased clearance of HMW multimers occurs as a result of increased binding of VWF to GpIb [Platelet-type 2B VWD will give similar results.] | ↓ VWF:CB and ↓ VWF:RCo |
| Type 2M | In Type 2M VWD HMW multimers are present despite defective platelet–VWF interaction, the VWF:CBA reflects the HMW VWF present and so is normal. |
Normal VWF:CB but ↓ VWF:RCo [VWF:RCo is lower than VWF:Ag (VWF:RCo/Ag ratio <0.7 but (VWF:CB/Ag ratio ‡ ~0.7] |
| Type 2N | Similarly in 2N VWD the VWF:CB will be normal as the multimeric structure of VWF is normal. | Normal VWF:CB and VWF:RCo |
| Type 3 | Type 3 VWD, there is no VWF and so the VWF:CB will be very low | ↓ VWF:CB and ↓ VWF:RCo |
Despite the limitations of the VWF:RCo assay, the VWF:CB assay is not a replacement for the VWF:RCo assay in the diagnosis and classification of VWD.
The VWF:RCo assay [assayed by platelet aggregometry] measures the ability of VWF in the presence of Ristocetin to interact with platelets via the GpIb-V-IX complex whereas the VWF:CB assay is a direct reflection of the ability of VWF to bind to collagen. Each of these assays measures a different function of the VWF molecule.
Both the VWF:RCo and the VWF:CB assay must be compared with the VWF:Ag
i.e. derive the VWF:RCo/VWF:Ag ratio and the VWF:RCo/VWF:Ag ratio.
Reference Ranges
The reference range for the VWF:CB assay is in the range of 50-194 U/dL.
What Test Next
The investigation of a patient with suspected VWD requires a number of assays including VWF:Ag, VWF:CB, VWF:RCo and FVIII:C. Its important to remember that 2N VWD is associated with normal or near normal VWF assays. 2N VWD should be considered in any individual with a low FVIII level. Historically a number of individuals with 2N VWD were diagnosed with mild Haemophilia A.
Finally it is important to remember that VWF levels vary significantly with ABO blood group and are 25% lower in individuals who are Blood Group O.
