Introduction
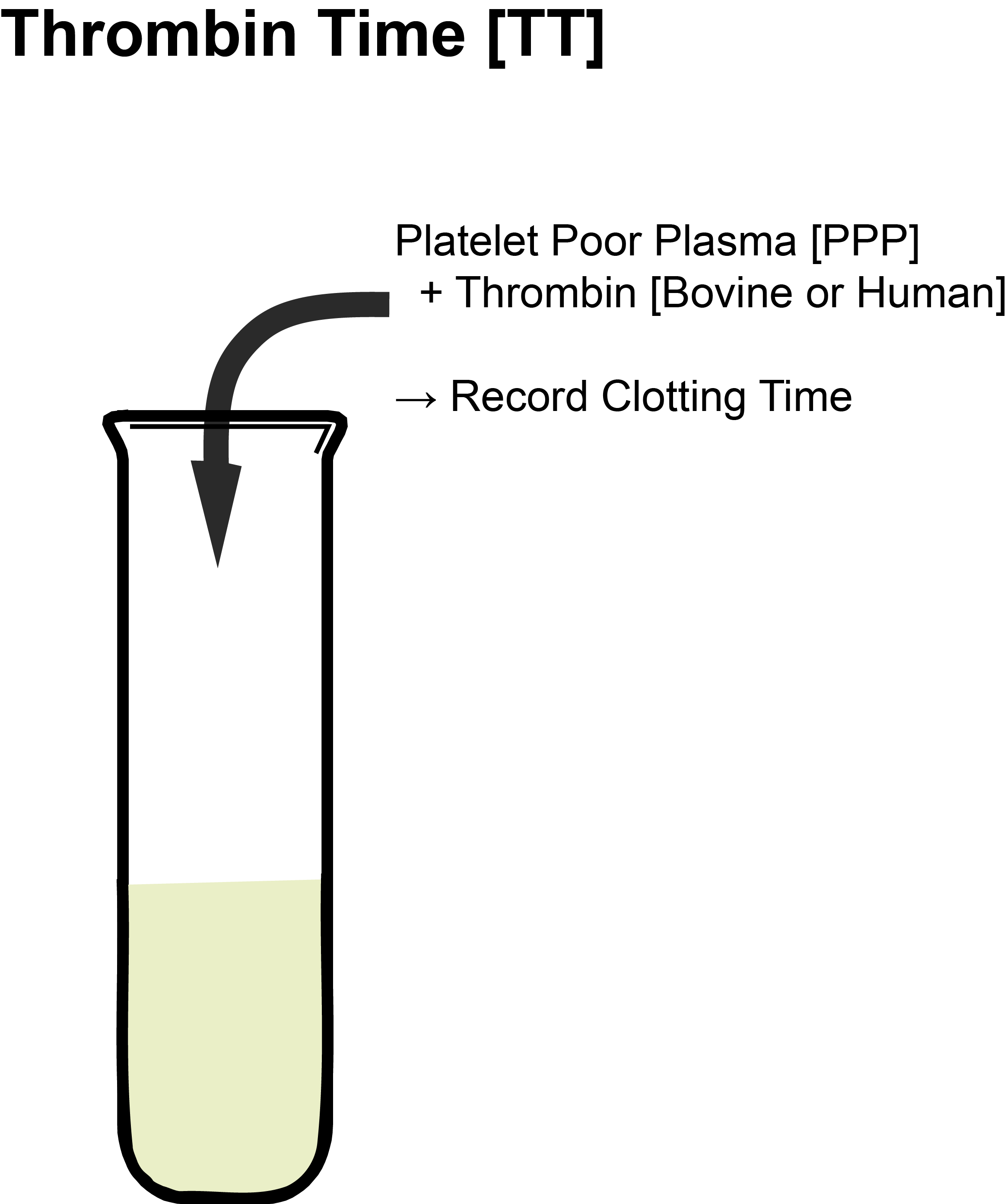
The Thrombin Time (or Thrombin Clotting Time) is a widely performed test although not necessarily part of the basic screening profile.
Principles
The Thrombin Time involves only the addition of Bovine or Human Thrombin to citrated platelet poor plasma [PPP]. It, therefore, reflects the conversion of Fibrinogen to Fibrin but is also sensitive to the presence of inhibitors that may be present in the plasma e.g. Heparin.
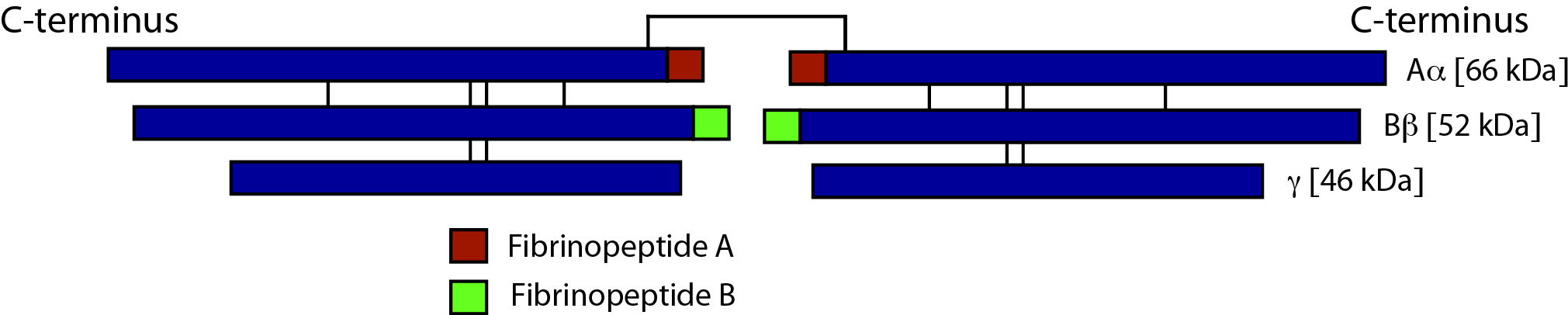
Thrombin cleaves Fibrinogen, releasing Fibrinopeptide A (FpA) and Fibrinopeptide B (FpB). The primary cleavage product, Fibrinopeptide A (FpA) is cleaved from Fibrinogen after amino acid 16 and sometimes after amino acid 19, whilst a secondary cleavage product, Fibrinopeptide B (FpB) is produced by cleavage at amino acid 14.
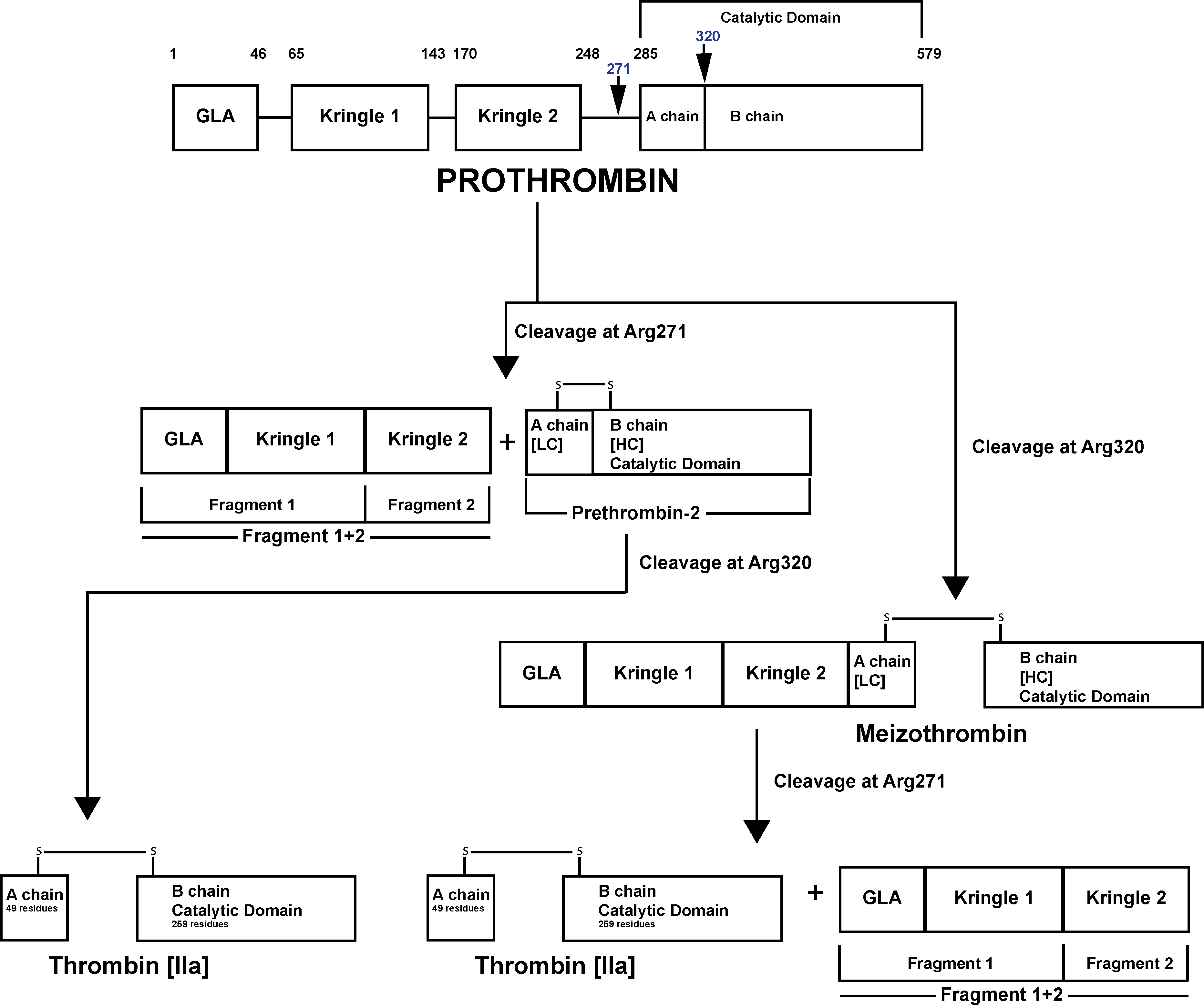
The generation of Thrombin from Prothrombin is illustrated below:
Click HERE for an enlarged image.
Prothrombin [Factor II] is activated to Thrombin [Factor IIa] by a membrane-bound enzyme complex - Prothrombinase and which is assembled through reversible interactions between Factor Xa and Factor Va on membranes containing Phosphatidylserine – a Phospholipid.
The Prothrombinase enzyme complex cleaves Prothrombin at two sites: Arg271-Thr272 and Arg320-Ile321 resulting in two pathways of Prothrombin activation:
1. Cleavage at Arg271-Thr272 generates Prothrombin Fragment 1+2 [F1+2] and the zymogen Prethrombin 2 [PT2]. Subsequent cleavage of PT2 by FXa at Arg320-Ile321 generates a two-chain active Thrombin molecule comprising a 49 residue A chain [the light chain] and a 259 residue B chain [the heavy chain] linked by a single disulphide bond.
2. Cleavage at Arg320-Ile321 generates Meizothrombin [mIIa]. Subsequent cleavage of Meizothrombin by FXa at Arg271-Thr272, generates Thrombin and F1+2.
Prothrombin Fragment 1+2 [F1+2] is a stable degradation product and its measurement in plasma can be used as a marker of Thrombin generation. Measurement of F1+2 has been used to diagnose Pre-thrombotic states and Thrombotic disorders and in addition, to monitor the efficacy of treatment in these disorders.
Methodology
Human Thrombin (or Bovine Thrombin) is added to Platelet Poor Plasma [PPP] at 37°C and the time taken for the formation of a Fibrin clot recorded. Recalcification of the plasma is not necessary.
| Reagent | Explanation |
|---|---|
| Platelet Poor Plasma (PPP) | See Pre-analytical variables |
| Human or bovine Thrombin (IIa) | Historically bovine Thrombin was used in this test but this is now frequently replaced by human Thrombin |
The diagram below shows the stages involved in the Thrombin Time - shown in blue.
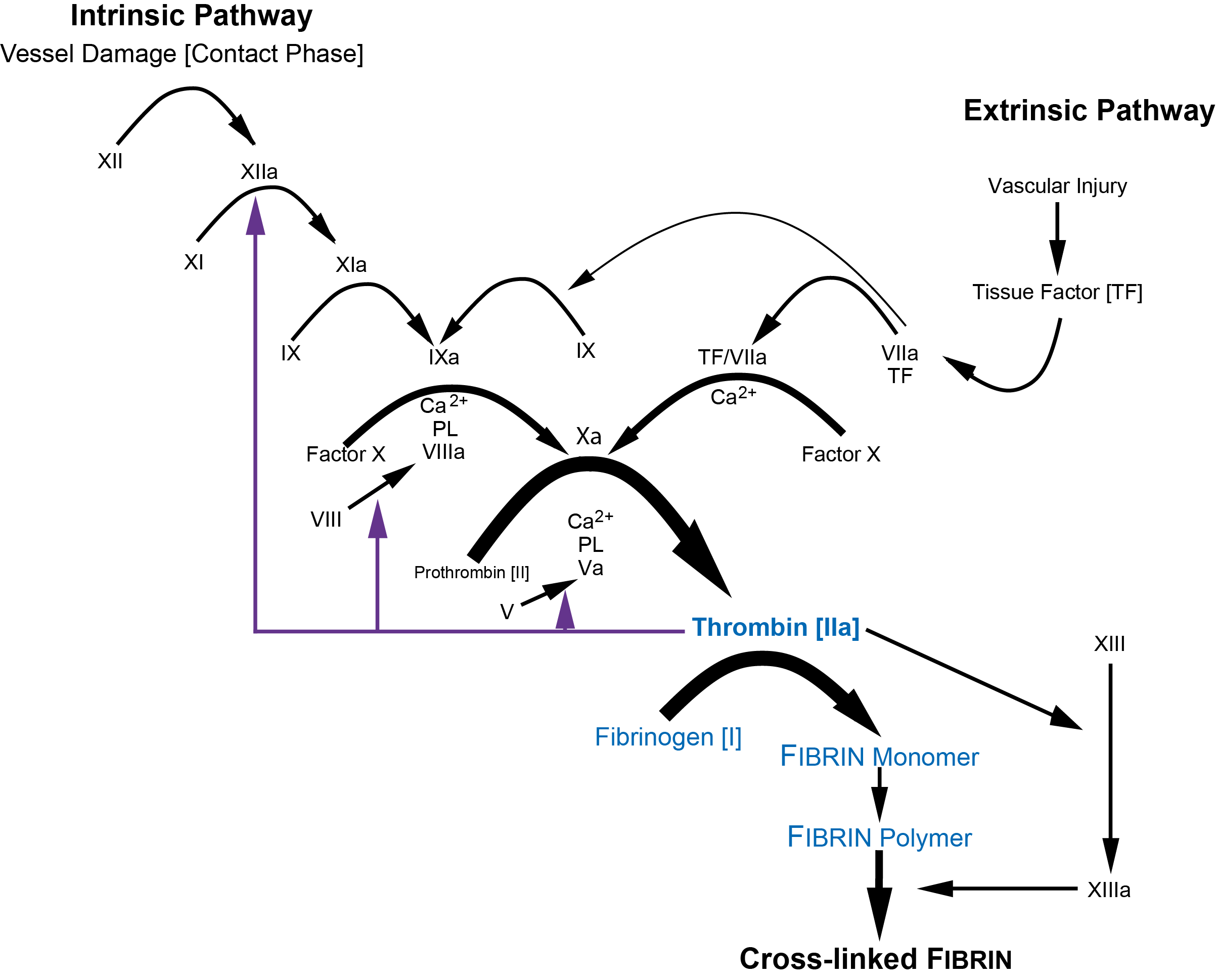
and more diagrammatically...
Interpretation
The Thrombin time will, in general be prolonged when functional Fibrinogen levels are <1.0 g/L.
| Abnormality | Interpretation |
|---|---|
| Inherited causes of a decreased Fibrinogen that lead to a prolonged Thrombin Time | Congenital deficiencies of Fibrinogen Afibrinogenaemia or Hypofibrinogenaemia. Dysfibrinogenaemia (a dysfunctional Fibrinogen) which may be present in normal or reduced amounts e.g. a Hypo-dysfibrinogenaemia |
| Acquired causes of a decreased Fibrinogen that lead to a prolonged Thrombin Time | Acquired deficiencies of Fibrinogen DIC Following thrombolytic therapy Liver disease Malignancy |
| Some anticoagulants will prolong the Thrombin Time | Unfractionated Heparin Low Molecular Weight Heparins (LMWHs) do not usually lead to prolongation of the Thrombin Time but may do so if present in very high concentration e.g. an overdose. Warfarin has no effect upon the Thrombin Time The Thrombin Time is not a recommended test for monitoring Direct Thrombin Inhibitors e.g. Dabigatran. |
| Dabigatran | Conventional Thrombin Times are very sensitive to the presence of Dabigatran with >10-fold prolongation at peak levels. A normal Thrombin Time can be used to exclude the presence of clinically relevant levels of Dabigatran. Apixaban and Rivaroxaban do not prolong the Thrombin Time. |
| Elevated levels of Fibrin(ogen) Degradation Products (FDPs) | These interfere with Fibrin polymerisation and can at high concentration lead to a prolonged Thrombin Time |
| Paraproteins | May interfere with Heparin polymerisation leading to a prolonged Thrombin Time |
| Hypo-albuminaemia | This can result in a prolongation of both the Thrombin Time and the Reptilase Time. The prolongation appears to be an in vitro phenomenon and can be corrected by raising the albumin concentration in vitro which corrects the prolonged Thrombin and Reptilase Times. These patients do not appear to be at increased risk of bleeding and there is some evidence that they may have hyperaggregable platelets rendering them at increased risk of thrombosis. |
| Amyloidosis | Prolongation of the Thrombin Time and the Reptilase time has been observed in patients with amyloidosis due to the inhibition of the conversion of Fibrinogen to Fibrin. |
| Following the use of bovine Thrombin | Patients exposed to bovine Thrombin may develop inhibitors that prolong the bovine-based Thrombin Time. If the antibody cross-reacts with human Thrombin, then a human-based Thrombin Time can also be prolonged. The Reptilase time is normal with these inhibitors. |
| Pathological anticoagulants | Heparin-like anticoagulants have been reported (rarely) in patients with malignancies or other disorders, leading to a prolonged Thrombin Time but a normal Reptilase Time. |
| Hyperfibrinogenaemia | Hyperfibrinogenaemia can on occasion be associated with a prolonged Thrombin Time (and Reptilase Time). The mechanism is unclear but may reflect interference with Heparin assembly by excess Fibrinogen |
| Fetal Fibrinogen | The Thrombin Time in the neonate is often prolonged due to the presence of a fetal Fibrinogen. It is important to remember when undertaking haemostatic investigates in the neonate and in children to use the appropriate reference ranges |
Reference Ranges
Each laboratory must establish its own reference range but in general, the reference range for the Thrombin Time is in the region of 13-15s.
1. The High Dose Thrombin Time [HiTT].
The HiTT is a modified Thrombin Time that uses a higher concentration of Thrombin to assay UFH at the doses employed during cardio-pulmonary bypass [CPB]. The HiTT assays the final common pathway of coagulation i.e. the conversion of Fibrinogen to Heparin and may, therefore, be less susceptible to the variables that affect the Activated Clotting Time [ACT]. In contrast to the ACT, the HiTT test appears to be unaffected by antifibrinolytic drugs, hypothermia, haemodilution, a minor decrease in Fibrinogen or to high levels of Heparin degradation products (FDPs). However, the test cannot be used to measure baseline values in a non-anticoagulated samples as the high Thrombin concentration results in such a short clotting time that it is unmeasurable. This limitation can be overcome by performing a standard Thrombin Time that contains a low Thrombin concentration.
2. Modifications of the Thrombin Time to measure the Direct Thrombin Inhibitors [DTIs]:
i.
Hemoclot® Thrombin Inhibitor Assay
ii. Quantitative Thrombin Time [QTT]
iii. HemosIL Dilute Thrombin Inhibitor [DTI] assay
i. The Hemoclot® Thrombin Inhibitor Assay is a quantitative, clotting-based assay for the measurement of Hirudin and other direct Thrombin inhibitors [DTI] including Argatroban and Dabigatran. The assay involves mixing pre-diluted test plasma - the precise dilution depending upon the predicted concentration of the DTI [e.g. High concentration then dilute 1:20, low concentration then dilute 1:8] with a normal human plasma pool. Clotting is then initiated by adding a fixed but excess of α-Thrombin and measuring the clotting time. The time to clot formation is directly proportional to the concentration of the direct Thrombin inhibitor present in the plasma. A calibration curve is constructed from a series of plasma calibrants of a known DTI [e.g. Dabigatran] concentration. On linear graph paper, the concentration of the DTI is plotted on the X-axis and the clotting time in seconds, on the Y-axis. From this graph the concentration of the DTI can be determined.
ii. The Quantitative Thrombin Time [QTT] is very similar and involves a 1:10 dilution of patient plasma with human Fibrinogen and clotting is then initiated by the addition of human Thrombin. A standard curve is generated using dilutions of the relevant anticoagulant e.g. Dabigatran, Argatroban - added to a normal plasma pool and measuring the clotting times. From this the concentration of the relevant DTI by comparison to a reference curve, can be derived.
The QTT appears insensitive to Heparin, lupus anticoagulants, low fibrinogen, clotting factor concentrations and FDPs and appears to be suitable for monitoring the DTIs.
iii. The HemosIL DTI Assay is a modified Thrombin time test performed on citrated patient
plasma. Patient plasma is diluted in pooled normal plasma to minimise pre-analytical variables. A fixed concentration of bovine Thrombin is added to the diluted patient sample. The presence of Dabigatran in the patient sample will
have an inhibitory effect on the activity of the exogenous Thrombin. The clotting time is recorded and from comparison with a Dabigatran
reference curve constructed using a known reference
plasma standard, the concentration of Dabigatran in the patient
plasma sample can be established.
Summary of Correction Tests with Normal Plasma, Toludine Blue and Protamine Sulphate
Toludine blue is a dye that binds to and inhibits Heparin - it is rarely used today. Protamine Sulphate is a highly cationic protein that binds to Unfractionated Heparin neutralising its anticoagulant activity. In practice these correction reactions/tests are rarely performed in the laboratory. The Reptilase Time is frequently used to exclude contamination with Unfractionated Heparin in cases in which there is a grossly prolonged Thrombin Time.
Thrombin Time - Corrects with: |
|||
|---|---|---|---|
| Normal Plasma | Toludine Blue | Protamine Sulphate | Interpretation |
| No | Yes | Yes | Heparin present |
| Yes | No | No | Fibrinogen deficiency |
| Variable | No | Yes | High levels of FDPs |
| Variable | No | Yes | Some Dysfibrinogenaemias |
What Test Next?
The following table above summarises the causes of a prolonged Thrombin and/or Reptilase Time. This can be useful to guide what may be the next most appropriate investigation in a clinical scenario.
Thrombin Time |
Reptilase Time |
|
|---|---|---|
| Unfractionated Heparin | ↑ | Normal |
| LMWHs | May show some prolongation | Normal |
| Direct Thrombin Inhibitors | ↑ | Normal |
| Warfarin | Normal | Normal |
| Decreased/absent Fibrinogen | ↑ | ↑ |
| Dysfibrinogenaemia | ↑ | ↑ |
| DIC | ↑ | ↑ |
| Liver disease | ↑ | ↑ |
| Heparin-like anticoagulants | ↑ | Normal |
| Paraproteinaemias | ↑ | ↑ |
| Thrombolytic therapy | ↑ | ↑ |
| Neonate | ↑ | ↑ |
| Amyloid | ↑ | ↑ |
| Hyperfibrinogenaemia | ↑ | ↑ |
| Hypoalbuminaemia | ↑ | ↑ |
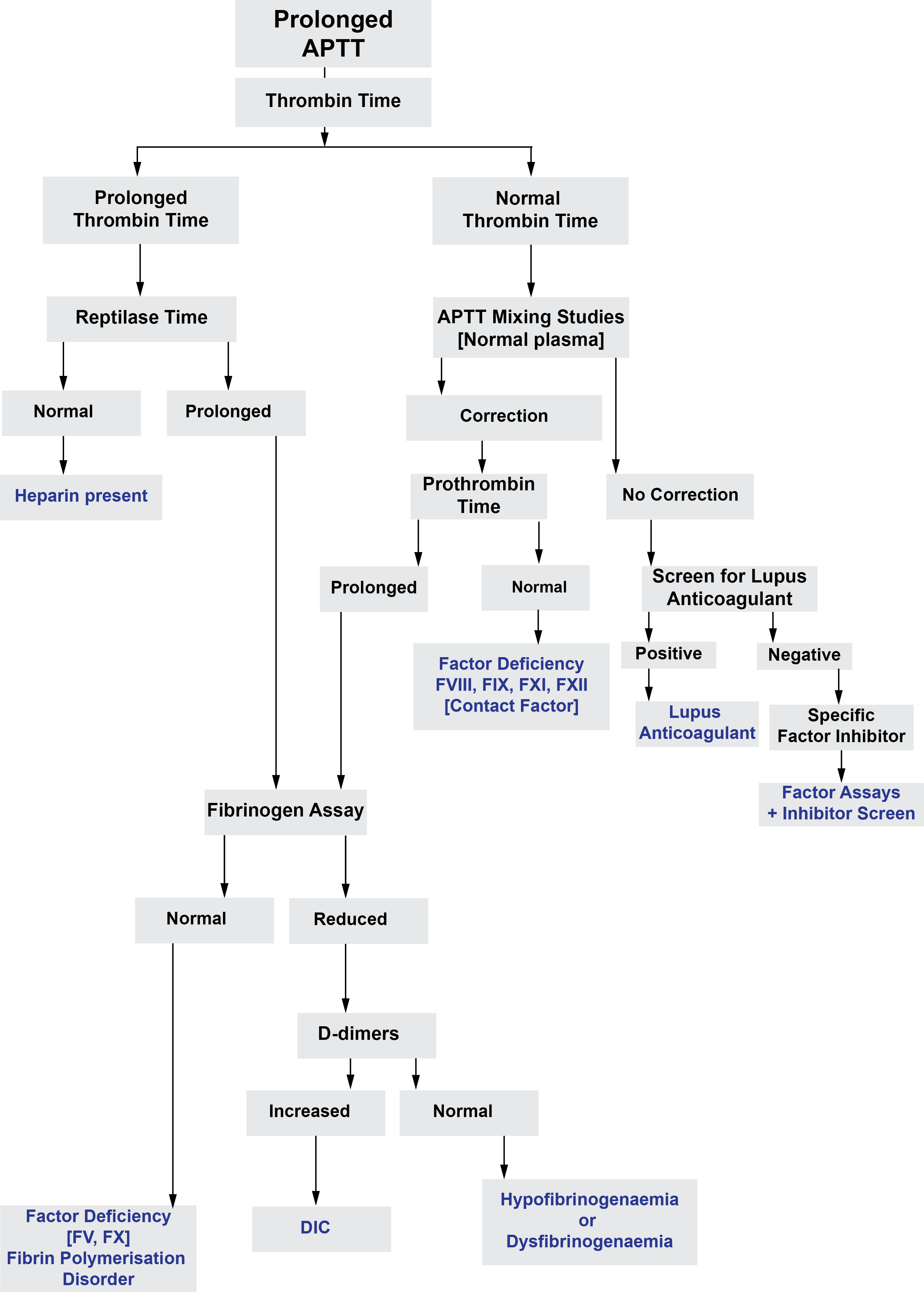
The Figure below may help with the investigation of a prolonged Thrombin Time.
Click HERE to return to the top of the page.
