Tissue-type Plasminogen Activator [t-PA] Assays
Introduction
t-PA (tissue-type Plasminogen Activator) is a serine protease and the main activator of Plasminogen to Plasmin (the other is urinary plasminogen activator: u-PA) and is, therefore, a vital component of the fibrinolytic system. T-PA is mostly found on endothelial cells where it acts to limit the propagation of clots in areas of intact vasculature.
T-PA is released continuously into the blood and is cleared equally rapidly by the liver. The T½ of t-PA is approximately 5 minutes. Activation of Plasminogen to Plasmin is slow/insignificant in the absence of a fibrin clot but fibrin strands offer binding sites for both Plasminogen and t-PA and bring t-PA and its substrate into close proximity at the site of clot formation. Binding of t-PA to fibrin increases its activity at least 1000-fold.
t-PA activity is inhibited by PAI-1 (plasminogen activator inhibitor-1) and most circulating t-PA is bound to this inactivator.
There are two forms of t-PA:
1. Single chain t-PA [sct-PA] - this is the native form of t-PA secreted from the endothelial cell.
2. Two-chain t-PA [tct-PA]. The activity of t-PA is significantly enhanced through proteolytic cleavage by Plasmin at Arg275-Ile276 to generate the two chain molecule.
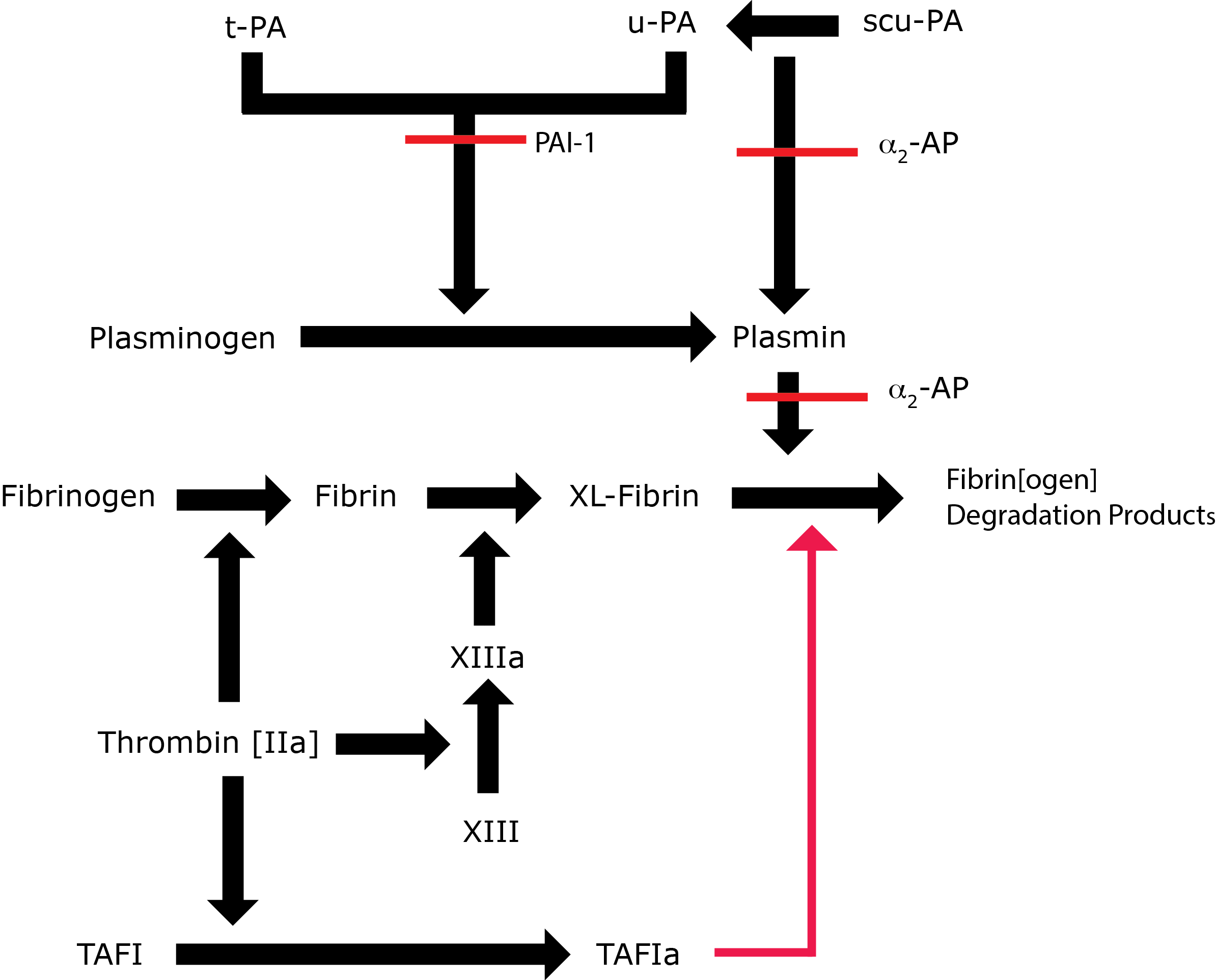
Key: t-PA - Tissue Plasminogen Activator; u-PA - Urokinase-type Plasminogen Activator; XL-Fibrin - cross-linked fibrin; TAFI - Thrombin Activatable Fibrinolytic Inhibitor; TAFIa - Activated Thrombin Activatable Fibrinolytic Inhibitor; α2-AP - Alpha-2-antiplasmin [Alpha2-Plasmin Inhibitor]; scu-PA - single chain Urokinase-type Plasminogen Activator. A red line indicates an inhibitory pathway.
Principles
Laboratory evaluation of t-PA levels is complicated by fluctuation of t-PA levels in blood (acute
phase reactant), as well as fluctuating levels of PAI-1 (acute phase reactant, diurnal variation), which
binds to and inactivates t-PA. A number of approaches to the assay of t-PA in plasma have been developed:
1.
An ELISA assay for t-PA has the advantage of being unaffected by the interaction of t-PA with its inhibitors e.g. PAI-1 and which may continue following sample collection.
2. A functional
Chromogenic (indirect determination through a plasmin-mediated reaction) or bio-immunoassay.
Method
1. Immunological Assays - Commercial kits are readily available for
measuring t-PA antigen.
2. Functional assay general points:
Fibrinolytic activity is influenced by multiple factors and accurate results of functional assays require maximal standardisation of blood collection. Typically samples should be taken from a rested, fasting subject in the morning with no consumption of cigarettes or alcohol in the hour beforehand. The sample should be taken into a tube containing reagents which prevents t-PA and PAI-1 complex formation in vitro.
a. Bioimmunoassay (BIA):
t-PA is complexed onto an immobilised monoclonal anti-t-PA at pH 6.0 After washing, any inhibitors are removed and the remainder of the assay proceeds at pH 7-8. Human Plasminogen and a chromogenic Plasmin substrate are added and then incubated at 37°C. The amount of colour change is measured photometrically and is proportional to the amount of t-PA present.
Acidification of the plasma prevents interference from any PAI-1 present.
b. Chromogenic assay:
These are similar in to the bioimmunoassay except that the t-PA is not antibody immobilised and a fibrin-like stimulator is usually added to augment Plasminogen conversion to Plasmin by t-PA .
The chromogenic assay may employ a synthetic substrate which is cleaved by t-PA
to generate the chromophore and this is then assayed by measuring the change in OD.
In producing a standard curve for calibration of the bioimmunoassay and functional chromogenic assays pooled human plasma and not recombinant t-PA should not be used as the latter does not give calibration curves suitable for assaying human t-PA .
Interpretation
ELISA Assays:
Provides a very reliable quantitation of total t-PA concentration although very high heparin concentrations may affect the assay.
Functional assays: The presence of other agents which lyse Plasminogen will interfere with the test. Heparin binds to t-PA and increases its activity.
These factors must be considered when interpreting results.
Abnormal tests should always be verified by repeat and abnormal levels should not be diagnosed on the basis of a single abnormal result.
t-PA activity levels are decreased during pregnancy but rise rapidly following delivery.
Anabolic steroids will increase t-PA activity. Similarly t-PA activity is elevated in patients with liver cirrhosis.
Interpretation of t-PA assays
| Overestimation of t-PA levels | Reduced t-PA activity | Reduced t-PA antigen | Elevated t-PA activity |
|---|---|---|---|
| Streptokinase, rt-PA and other lytic agents
Heparin [the heparin-tPA complex has increased plasminogen activation activity] |
Alcohol [increases PAI-1 levels] Smoking [increases PAI-1 levels] |
Some dietary factors | Alcohol [rebound increase in activity ~12 hours later] DDAVP Exercise Insect venom in patients allergic to venom Physiological and psychological stress Oral contraceptives Venous occlusion Pregnancy Anabolic steroids Liver cirrhosis |
Reference Ranges
Local normal ranges should be determined in general are in the region of:
t-PA antigen 1-20 ng/ml
t-PA activity 0.2-2 IU/ml
What Test Next?
In cases of suspected disordered Fibrinolysis, the TEG-ROTEM can be very useful as a global assessment of Fibrinolysis. Sequence analysis of the relevant genes is also fundamental to the investigation of someone with suspected disordered Fibrinolysis.
