Anti-Platelet Factor 4 [PF4] Assays
Introduction
There are two types of Heparin Induced Thrombocytopenia [HIT] - Type I and Type II.
| HIT Type | Features |
|---|---|
| I | This is caused by a direct aggregating effect of heparin on platelets and leads to a mild transient thrombocytopenia. The platelet counts usually falls within the first 2-3 days after the start of heparin therapy and usually takes approximately the same time to recover when the heparin is stopped. The platelet count rarely falls below 100 x 109/L. |
| II | This is an immune-mediated disorder in which heparin binds to Platelet Factor 4 [PF4] - a protein present in plasma. This leads to the formation of IgG anti-PF4–heparin antibodies and the formation of IgG heparin–PF4 immune complexes. The antibodies can bind to the Fc receptor on platelets leading to platelet activation. In addition the immune complexes interact with monocytes and endothelial cells inducing tissue factor expression and damage to the endothelial cells. The net effect is a highly prothrombotic state. The platelet count usually falls within 5-14 days of the start of heparin but may fall more rapidly in individuals who have been previously exposed to heparin and who have developed anti-PF4–heparin IgG antibodies. The antibodies are frequently undetectable after 100 days. After the heparin is stopped the platelet counts usually start to rise within 2-3 days and usually normalise within 10-14 days. Type II HIT usually results in moderate to severe thrombocytopenia, with platelet counts commonly <100 x 109/L. |
The '4T' scoring system of Warkentin [see References] is widely used to predict the risk that an individual with thrombocytopenia may have HIT.
4T Scoring system for Suspected HIT
| 'T' | SCORE | ||
|---|---|---|---|
| 2 | 1 | 0 | |
| Thrombocytopenia | >50% fall in platelet count or a platelet nadir of 20-100 x 109/L | 30-50% in platelet count or a platelet nadir of 10-19 x 109/L | <30% fall in platelet count or a platelet nadir of <10 x 109/L |
| Timing | Onset with 5-10 days of exposure to heparin or <1 day if previous exposure to heparin within 100 days |
Unclear - Platelet count falls after 10 days |
Platelet count falls too early and without recent exposure to heparin |
| Thrombosis | New thrombosis Skin necrosis |
Progressive or recurrent thrombosis Some skin lesions e.g. erythema |
None |
| Other causes of Thrombocytopenia are not evident | No other cause identified | Possible other cause | Other cause clearly identifiable |
A score of ≤3 indicates a low pretest probability for Type II HIT [<5% chance of HIT]
A score of 4–5 indicates an intermediate risk.
A score ≥6 is associated with a very high risk of HIT.
The American College of Chest Physicians (ACCP) Guidelines for the diagnosis of Type II HIT has identified the following diagnostic criteria:
1. Thrombocytopenia - a fall in platelet count that occurs 4–10 days after beginning heparin therapy
2.
A fall in platelet count to <150 x 109/L or to <50% of the baseline platelet count
3. The
exclusion of other causes of thrombocytopenia
4. The recovery of the platelet count to >90% of the baseline platelet count after heparin is stopped.
Remember not all patients with HIT will develop a thrombosis. The following diagram illustrates this:
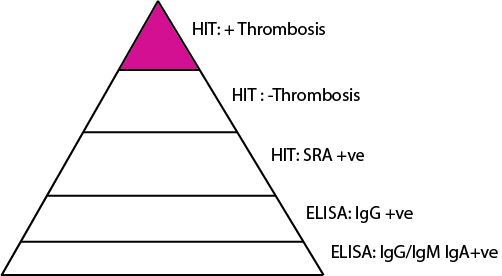
A significant number of individuals may have a positive ELISA assay that detects a variety of antibodies some of which are non-pathological but only a small number will have clinically significant HIT.
Principles & Methods
A number of tests exist for the detection of antibodies in suspected cases of HIT and these can be either functional tests or immunological tests.
| Test | Method |
|---|---|
| 1. Platelet aggregation | Heparin induced platelet aggregation is the easiest functional test to perform and is most commonly used; however, the sensitivity of heparin induced platelet aggregation is only 35–85%. Donor selection is important as platelet responsiveness to HIT antibodies varies. HIT antibodies produce activation of platelets at 0.1 - 0.3 IU/ml heparin and this is abolished at high heparin concentration [100 IU/mL.] The sensitivity of the test can be increased by using washed platelets but this is technically demanding. A variety of platelet activation endpoints can then be used, including release of radioactive serotonin. |
| 2. 14C-Serotinin Release Assay [SRA] | [14C] serotonin release assay [SRA] in which donor platelets loaded with [14C] serotonin are mixed with heparin and patient serum and the percentage of serotonin released is measured. The SRA is 95% sensitive and specific but the test is technically complex and less readily available. |
| 3. PF4 ELISA Assay | The anti-heparin–PF4 ELISA is a commercially available standardised test that detects heparin antibodies bound to the PF4–heparin complex. The sensitivity of this test is approximately 80–100%; however, specificity is low due to potential cross-reacting antibody detection. If positive, the PF4 ELISA can be repeated using high-dose heparin (100 U/mL). Inhibition of a positive result (>50% reduction in the optical density) is characteristic of HIT antibodies. |
| 4. Flow Cytometry Assay | A less commonly used functional test is the flow cytometric assay which detects platelet microparticle release. |
| 5. Latex-based method | This uses a monoclonal antibody that mimics human HIT antibodies and is coated onto latex particles. In the presence of PF4 from human platelets complexed to polyvinyl sulfonate and the patient sample, a competitive agglutination reaction occurs. The degree of agglutination is inversely proportional to the concentration of antibodies in the sample and is determined by measuring the decrease of transmitted light caused by the aggregates. |
| 6. Heparin-induced Platelet Activation [HIPA]s | The washed-platelet Heparin-induced Platelet Activation (HIPA) test is a functional assay that detects clinically significant heparin antibodies. The HIPA has the same sensitivity and specificity for heparin-associated antibodies as the 14C-Serotinin Release Assay). |
Interpretation
1. HIT assays should be interpreted in the context of all the clinical information including the platelet count, the type of heparin and the duration of heparin exposure, previous heparin exposure and any thrombotic history. The 4T scoring system is invaluable.
2. The PF4 ELISA assay is frequently used to screen for HIT
but the OD reading is vital. The following tables give the likelihood of a diagnosis of HIT based on the SRA using the OD cut-offs for the ELISA assay.
| OD [Units] | Interpretation |
|---|---|
| <0.40 | 0 |
| 0.40–<1.00 | <5% |
| 1.00–<1.40 | ~20% |
| 1.40–<2.00 | ~50% |
| >2.00 | >90% |
For every increase of 0.5 OD units the risk of a strongly positive SRA result is increased by 6.3 fold. For an increase of 1.00 OD units the risk is increased by ~41-fold.
Reference Ranges
There is no reference range for this test. Remember although HIT antibodies may be detectable they are not necessarily pathogenic - see above.
