Introduction
The Prothrombin Time was described by Quick in 1935 and the test was initially often referred to as 'Quick's Prothrombin Time.' The Prothrombin Time was developed to measure Prothrombin (Factor II) and from which its name originated. However, it subsequently became clear that it was sensitive to abnormalities of Factors VII, X, V, II [Prothrombin] and Fibrinogen [Factor I].
A number of modifications of the PT have been made to make it more specific for the Vitamin K dependent clotting factors - covered below.
The Prothrombin Time (PT) in contrast to the APTT, measures the activity of the so-called Extrinsic and Common pathways of coagulation. The division of the clotting cascade into the Intrinsic, Extrinsic and Common pathways is artificial and has little in vivo validity but nevertheless remains a useful concept for interpreting the results of laboratory investigations.
The Prothrombin Time is a one-stage test based upon the time required for a Fibrin clot to form after the addition of Tissue Factor (TF - historically known as Tissue Thromboplastin), Phospholipid and calcium to de-calcified, platelet poor plasma [PPP].
The term 'Thromboplastin' was originally used to describe a substance in plasma that converted Prothrombin to Thrombin. Historically thromboplastins were extracted from brain and other organs and these contained significant amounts of Tissue Factor [TF] and Phospholipid [Pl]. TF is species specific and most laboratories now use a recombinant human TF with an International Sensitivity Index [ISI] close to 1 and which is relipidated to provide a source of Phospholipid. Animal thromboplastins are usually derived from rabbit brain.
Tissue Factor [TF] was originally designated Factor III [FIII] when the nomenclature of the clotting proteins was undertaken.
Principles
The PT measures the activity of the so-called extrinsic and common pathways of coagulation and therefore, is dependent on the functional activity of factors VII, X, V, II (Prothrombin) and Fibrinogen. The diagram below shows the clotting cascade - the factors that affect the Prothrombin Time are shown in blue.
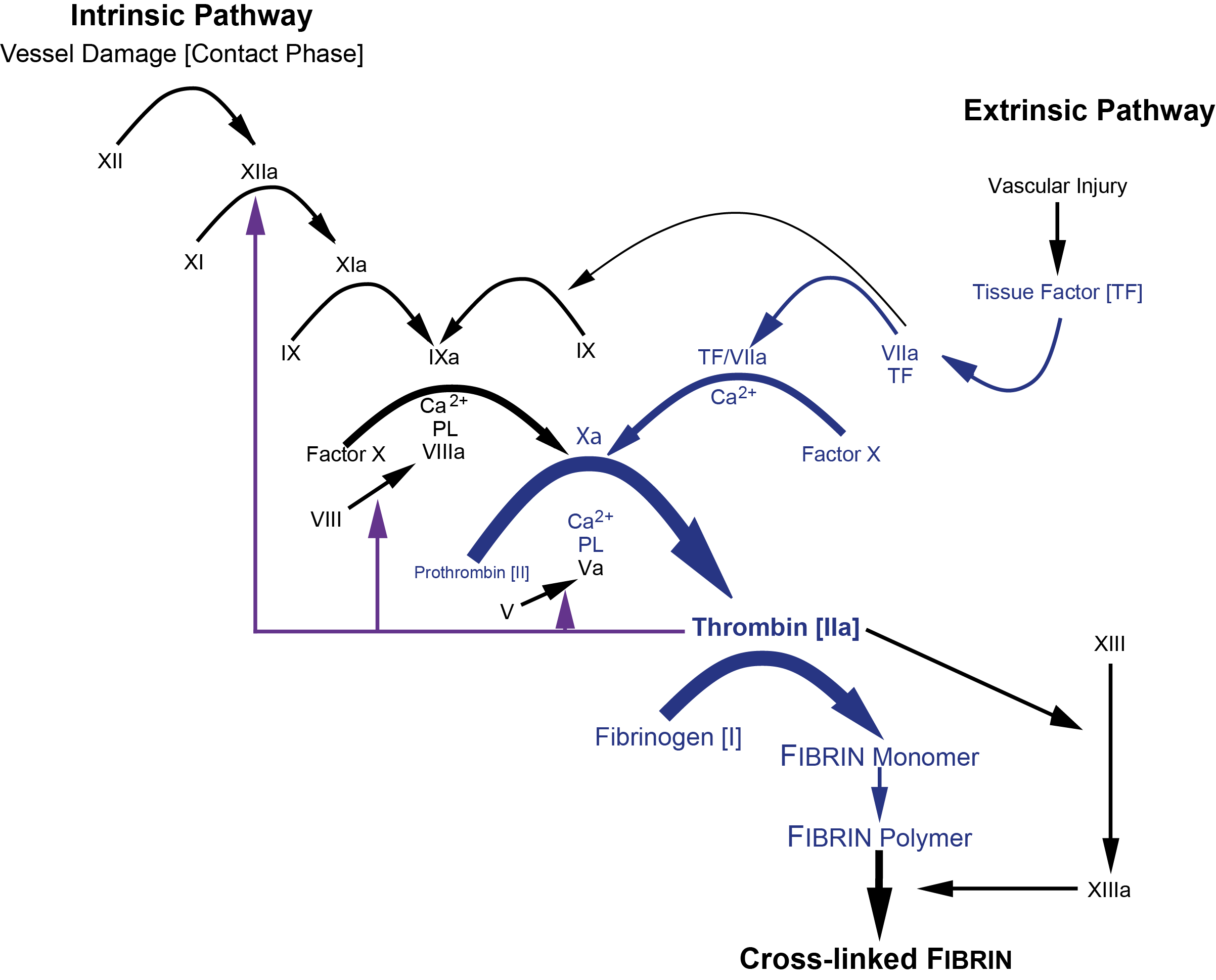
or more diagrammatically...

Method
Platelet poor plasma [PPP] is mixed with Tissue Factor (TF) (containing phospholipid) at 37°C and an excess of Calcium Chloride (25mM) is added to initiate coagulation. In the manual technique at the same time as the calcium is added, a stopwatch is started and stopped when the clot forms. The time taken from the addition of calcium to the formation of the Fibrin clot is known as the Prothrombin Time or PT. In an automated system the formation of the clot is detected electronically but the principles are identical.
| Reagent | Explanation |
|---|---|
| Platelet Poor Plasma (PPP) | See Pre-analytical Variables |
| Tissue Factor [containing Phospholipid] | Tissue Factor binds to FVII and initiates coagulation. Exogenous phospholipid is used to replace platelet phospholipid |
| Calcium | Required for re-calcification [- remember the plasma sample is citrated to inhibit clot formation when the blood sample is collected] |
Interpretation
The PT is usually performed as part of a series of tests which will include the APTT and sometimes the measurement of Fibrinogen levels and possibly a Thrombin time.
| Abnormality | Interpretation |
|---|---|
| Isolated Prolonged PT | Factor VII deficiency |
| Prolonged PT in association with other coagulation abnormalities | Vitamin K deficiency Vitamin K antagonists e.g. Warfarin, phenindione, rodenticides Liver disease Malabsorption (leading to vitamin K deficiency) High concentrations of unfractionated heparin Direct thrombin [IIa] inhibitors e.g. Lepirudin, Argatroban, Dabigatran Factor Xa inhibitors - DOACs Afibrinogenaemia and dysfibrinogenaemia Dilutional coagulopathy e.g. massive blood transfusion Multiple clotting factor deficiencies e.g. FV and FVIII deficiency Abnormalities of the vitamin K cycle e.g. mutations within the VKORC1 gene Chromosomal aberrations - the F7 and F10 genes are located on the long arm of chromosome 13 - deletions of which are associated with reduced FVII and FX levels. |
| Shortened PT | Following treatment with rVIIa [NovoSeven] |
Reference Ranges
The reference range depends upon a number of variables including:
- Source of Tissue Factor e.g. human, rabbit etc
- The exact technique used e.g. manual or automated
- Method of end-point determination e.g. optical or mechanical
Each laboratory should establish its own normal range but in general the Prothrombin time for a normal plasma sample, lies between 13-15 seconds.
In this modification of the Prothrombin Time, Factor II and Factor X are removed from pooled normal Platelet Poor Plasma [PPP] by double immunodepletion (Fiix-depleted plasma). The Fiix-depleted plasma is then mixed with test plasma and this corrects for any clotting factor deficiencies other than that of Factors II or X in the patient sample. Thromboplastin is then added which contains Tissue Factor and Phospholipid. Coagulation is initiated by the addition of Calcium and the clotting time measured.
The test is designed to monitor Vitamin K antagonists such as Warfarin but more recent data suggests that it may be suitable for monitoring the DOACs including Dabigatran, Rivaroxaban and Apixaban.
In the Owren Prothrombin Time, the plasma sample is diluted both to increase the sensitivity of the test but also to minimise any effect that heparin may have on the PT. In addition bovine Factor V is added from which Prothrombin [Factor II] and Factor VII have been removed, as a source of Fibrinogen and Factor V.
Therefore, the Owren Prothrombin Time is sensitive only to the activity of coagulation Factors II, VII and X.
Patient Platelet Poor Citrated Plasma is diluted 1 in 10 with buffer and thromboplastin [prepared from brain extract and so is a source of both Tissue Factor [TF] and Phospholipid [PL]] and bovine plasma is added and incubated at 37C. Calcium is added to initiate clotting and the time to clot formation measured.
What Test Next?
In cases in which there is an isolated prolongation of the PT and the remainder of the screening tests (APTT, TT and Fibrinogen) are normal - the next most logical test is a Factor VII assay.
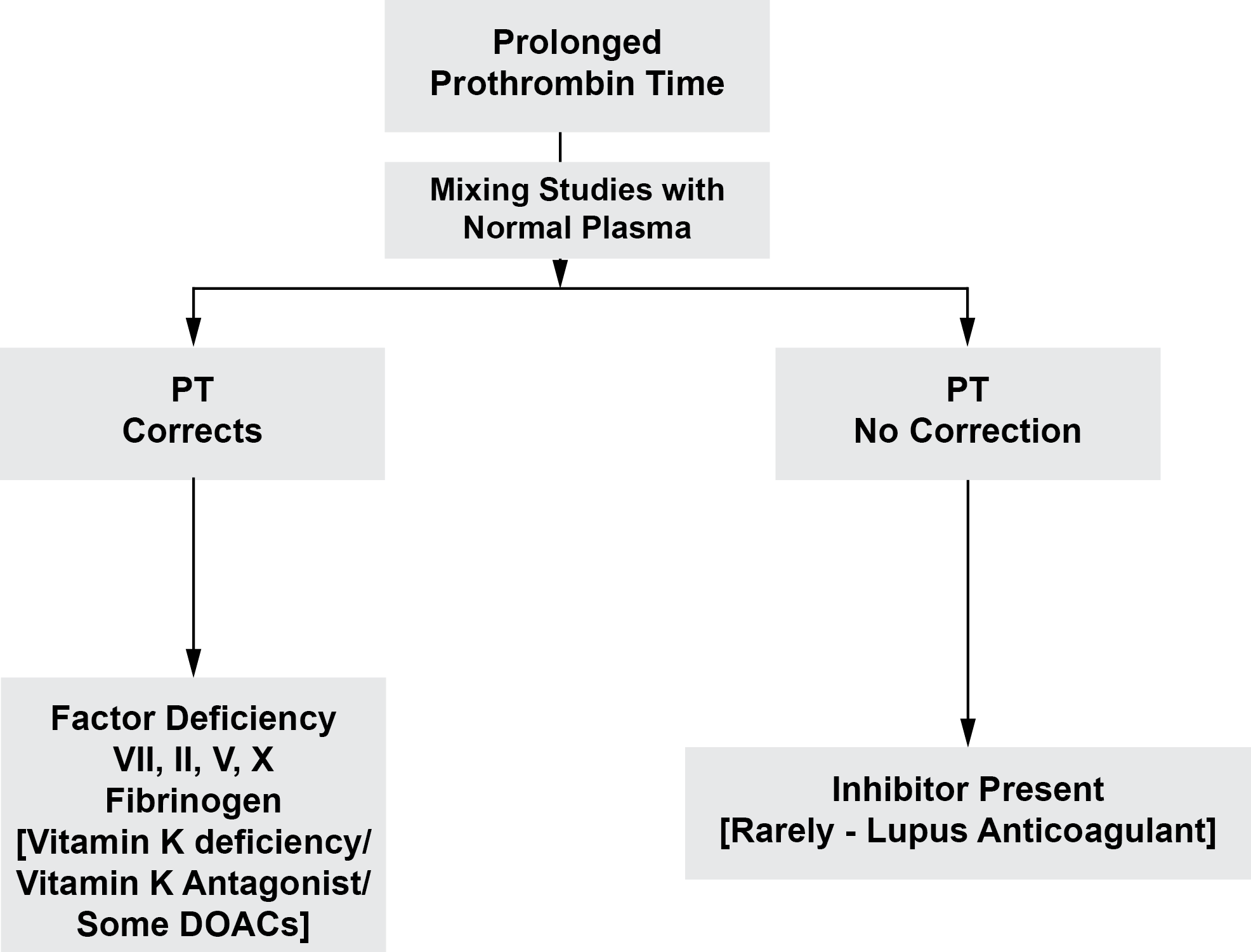
Factor VII deficiency is rare and it is more common to find a prolonged PT in combination with other abnormalities of the screen e.g. a prolonged APTT. In these cases - consult the table above and the figure below, for the possible differential diagnoses and therefore, how to proceed with further investigation. The history including a drug history and the examination are of fundamental importance
Remember - Warfarin and other oral Vitamin K antagonists will significantly prolong the PT but may prolong the APTT by only a few seconds (except in overdose).
The flow chart below shows how to investigate a prolonged PT.
Click HERE to return to the top of the page.
