Kaolin Clotting Time [KCT]
Introduction
The Kaolin Clotting Time (KCT) has often been regarded as the most sensitive test for the detection of circulating anticoagulants. The KCT detects all class of inhibitors, including those directed against Factor VIII but is also sensitive to the presence of Unfractionated Heparin [UFH].
Principles
The Kaolin Clotting Time (KCT) is essentially an Activated Partial Thromboplastin Time test but without any added phospholipid. The test relies on residual cell membrane fragments and plasma lipids to provide a Phospholipid surface for coagulation reactions.
Method
Dilutions of Normal:Patient plasma are prepared as shown in the table below. Kaolin is added and then calcium to initiate coagulation. The KCT is the time from adding calcium to clot formation. Kaolin suspension is turbid making it difficult to use optical density measurements to determine the endpoint and therefore usually requires the test to be performed manually. However, recently less turbid kaolin suspensions have been developed, permitting automation of the test.
| Normal Plasma | Patient Plasma |
|---|---|
| 100% | 0% |
| 90% | 10% |
| 80% | 20% |
| 50% | 50% |
| 20% | 80% |
| 10% | 90% |
There is no phospholipid correction step for the KCT. Instead factor deficiencies as an alternative explanation for a prolonged KCT are excluded by repeating the test with the addition of relatively large quantities of normal plasma. This will shorten the KCT by replacing any deficient clotting factor but in the presence of a coagulation inhibitor there will be no or limited correction. Similarly unfractionated heparin can usually be excluded by establishing whether the patient is on heparin or not [the thrombin time and reptilase time may be useful.]
The initial steep slope of the KCT [see the Type 1 curve below] is very important and allows the test to be simplified and used as a screening test. A test comprising 100% normal plasma and 80% normal:20% patient plasma is used and a ratio derived using the formula:
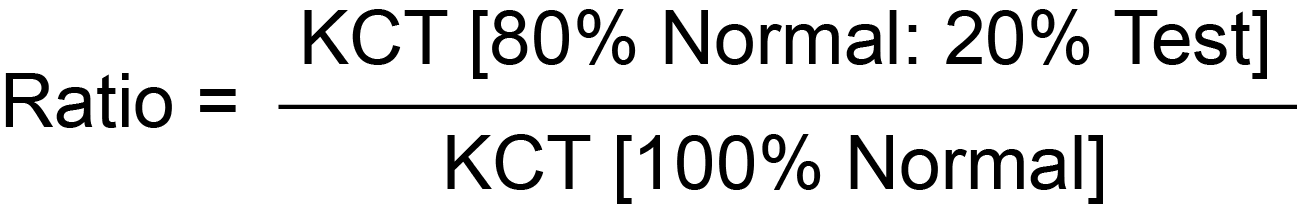
A ratio of ≥1.2 is considered positive for a Lupus Anticoagulant although reference ranges should be established locally.
Rosner Index/Chang Percentage: The Rosner Index and Chang
Percentage take into account the
degree to which the APTT corrects in a mixing study relative to the patient's initial [prolonged] clotting
time. Whereas the Rosner Index
is based on a 1:1 mix, Chang &
colleagues found that the 4:1 mix
increased the sensitivity of the test. It is important to remember that these formulae will be abnormal in a plasma that has a clotting factor deficiency or a Lupus Anticoagulant.
Rosner Index:
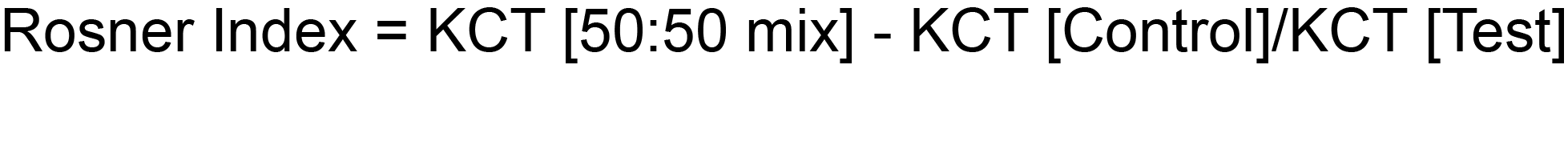
The normal range for the Rosner Index is <0.15. The Rosner is sometimes converted into a percentage.
A normal plasma has a value <15% and a positive test is >15%.
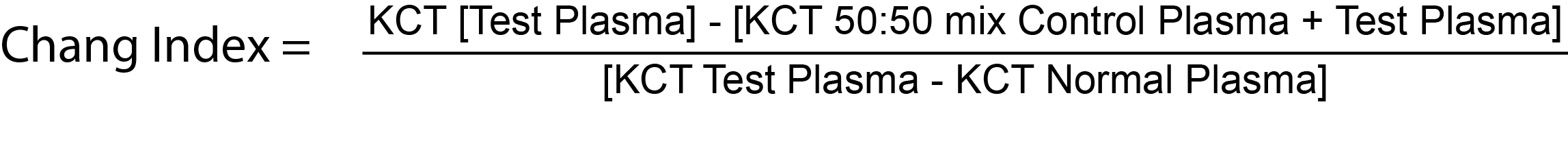
Chang Percentage:
In the original test Chang and colleagues proposed the following correction formula in which there was a 50:50 mix of the test plasma with control plasma:
But in a subsequent paper, they suggested that the sensitivity of the test could be improved [whilst maintaining the specificity] by using a 4:1 mix of test plasma to control plasma
[this avoids 'swamping' a weak LA with normal plasma] and appears to improve both specificity and sensitivity:
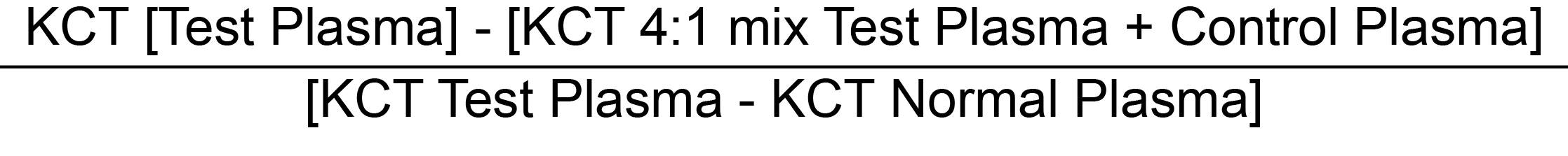
The Chang index is converted into a percentage correction by multiplying the final result by 100.
1.
In the original test using a 1:1 [50:50] mix of test plasma and control plasma, a positive result [i.e. Lupus Anticoagulant present] was a percentage correction >70% and a borderline result between as between 58-70%.
2.
In the modified test using a 4:1 mix of test plasma and control plasma, a test was considered positive if the percentage correction was >50%.
Interpretation
The KCT relies on small quantities of phospholipid in the patientís plasma and so is particularly sensitive to platelet contamination of the plasma sample, which greatly reduces the sensitivity of the test, especially after freezing and thawing, which disrupts platelet membranes and creates a large surface area for coagulation. A KCT of <60 s suggests contamination of the normal control plasma with platelet fragments and invalidates the result.
The KCT of a test sample is compared to that of a control. A test/control ratio of ≥1.2 indicates an inhibitor (1.1-1.2 is considered equivocal). Factor deficiency may be distinguished from APL by the addition of large amounts of normal plasma which will correct the prolonged KCT in factor deficiency but not with APL.
If the clotting times for the various plasma dilutions are plotted on Lin-Lin paper, a series of curves [Types 1-4] can be generated which are shown below:
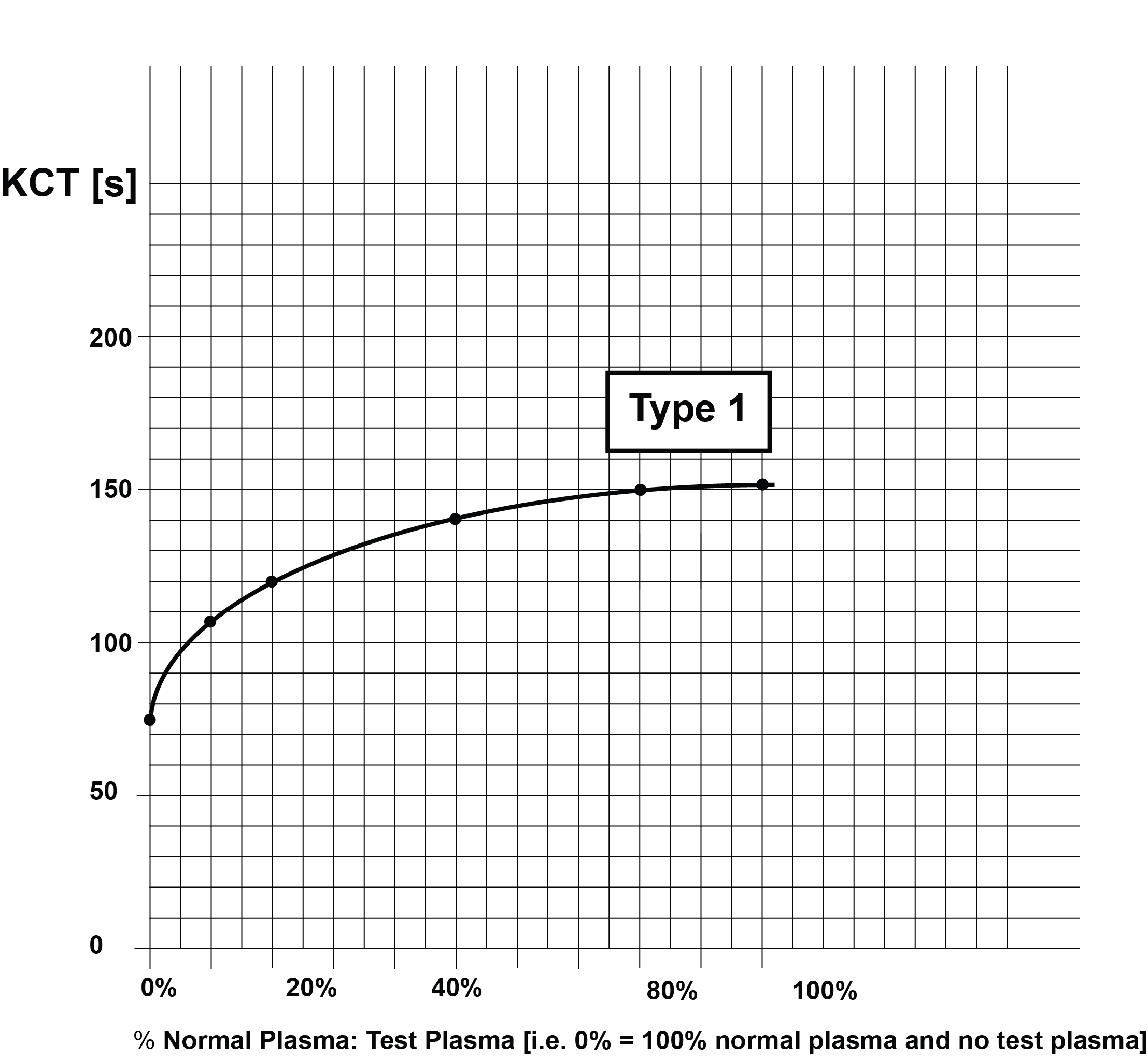
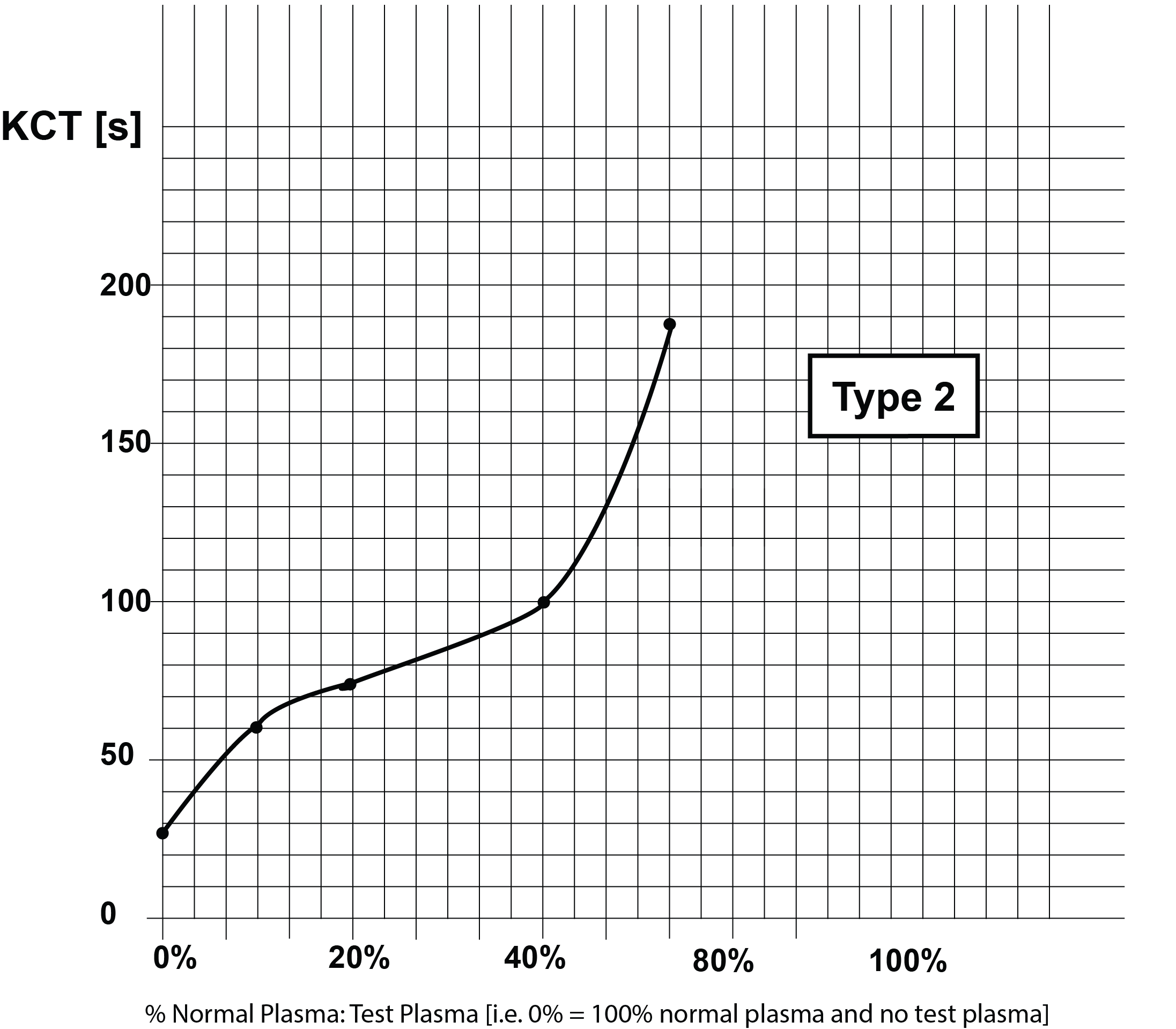
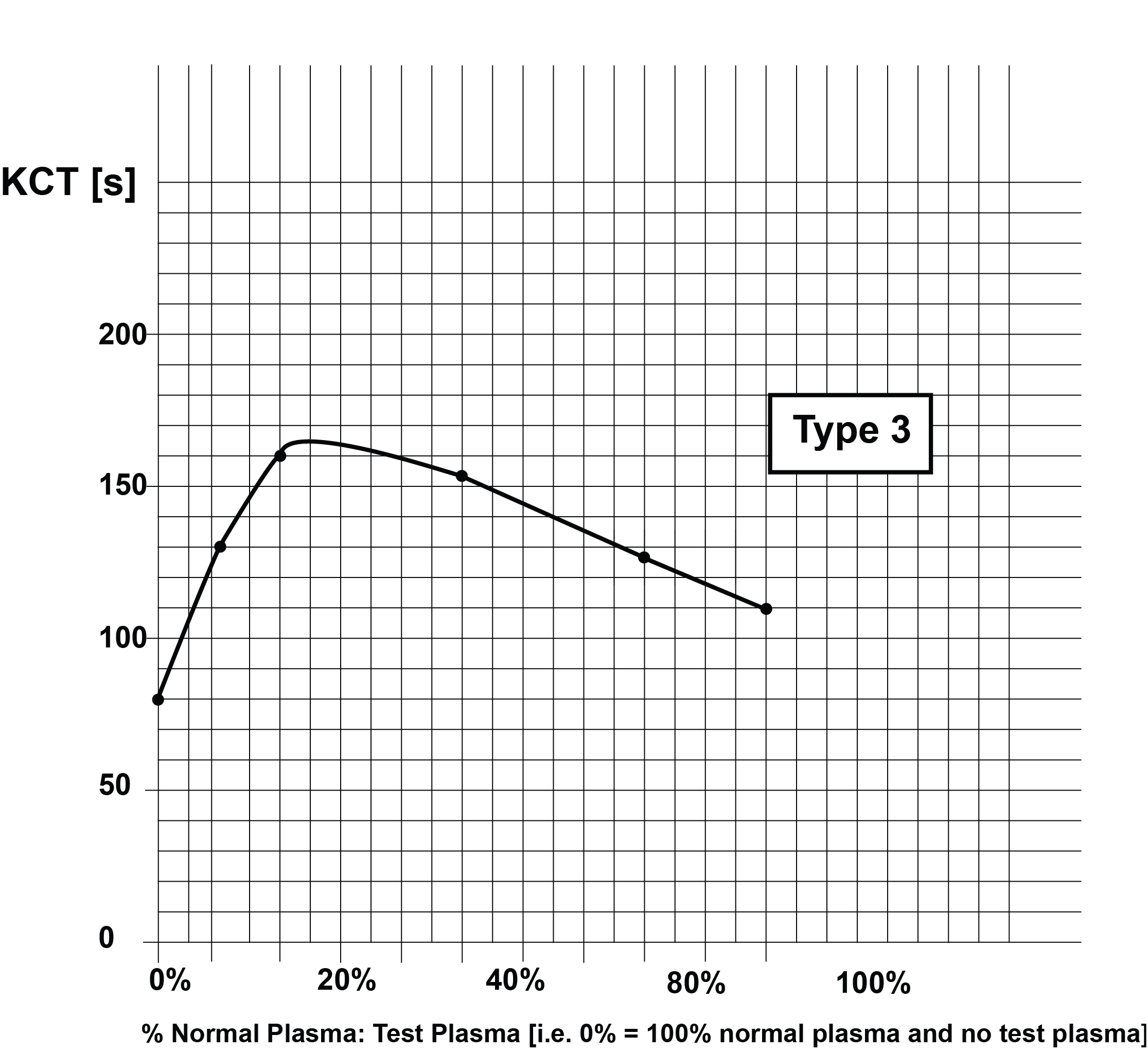
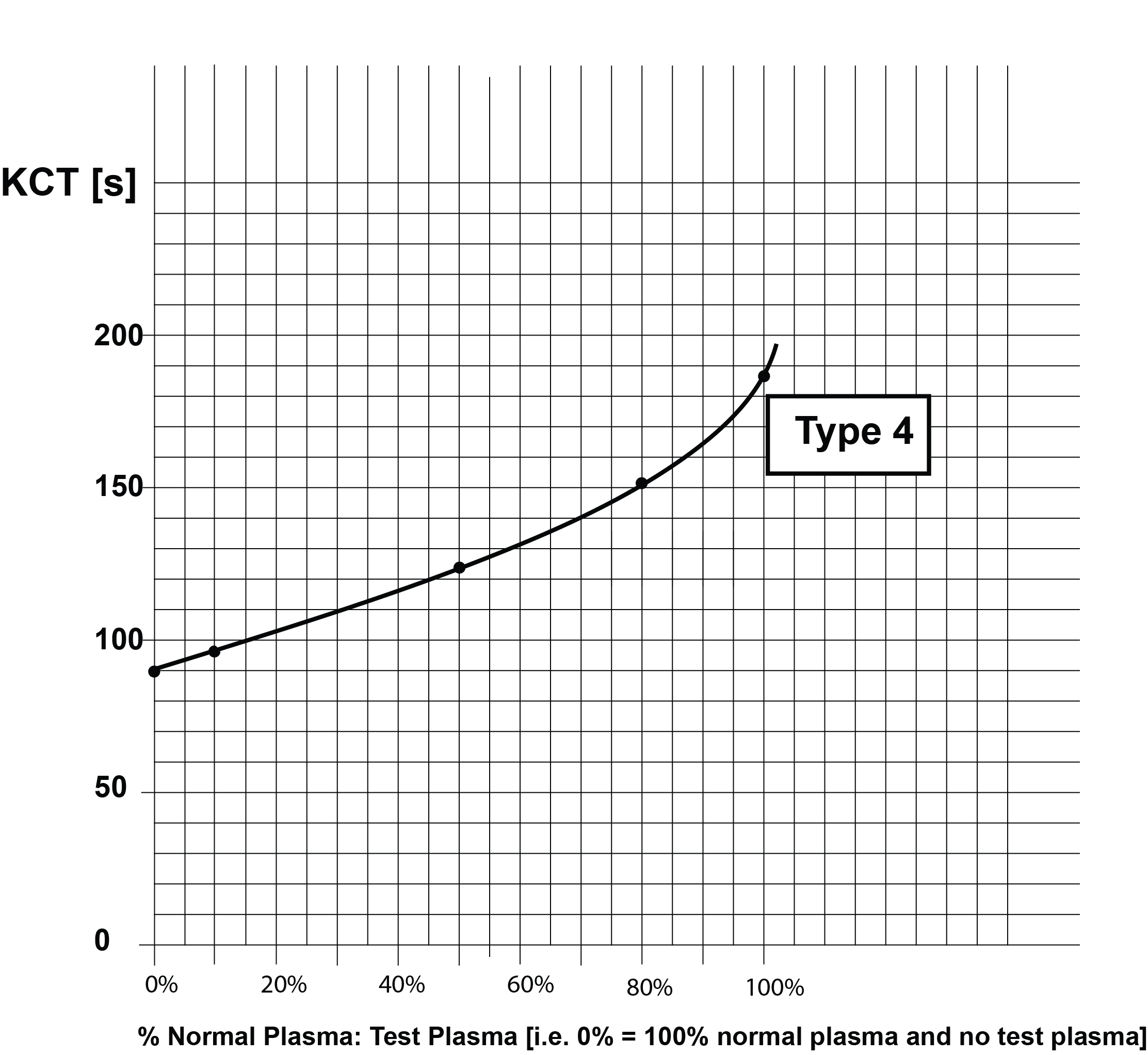
These curves are summarised in the following table:
KCT Curves: Summary
| Curve | Interpretation |
|---|---|
| Type 1 | Lupus anticoagulant present i.e. a positive result. The KCT of normal plasma is the 0% dilution on the X axis i.e. no patient plasma is present. This should be in excess of 60s otherwise the normal plasma contains too high a concentration of PL and looses sensitivity. Remember in the KCT the only source of PL in the test |
| Type 2 | Lupus anticoagulant present + a clotting factor deficiency |
| Type 3 | Lupus anticoagulant present but deficient in β2-GPI i.e. an anti-β2-GPI antibody is present |
| Type 4 | No Lupus Anticoagulant present i.e. a negative result |
Reference Ranges
See text above
What Test Next
In individuals in whom a LA is identified, the test should be repeated in 12 weeks. It should also be remembered that not all tests including the dRVVT or the SCT will identify all LAs and therefore, if the index of suspicion is that a specific patients has a LA then other tests should be undertaken. Finally - the causes of a LA should be screened for.
