Introduction
Antiphospholipid antibodies (APL) disrupt the coagulation process and are important for two reasons:
1. A Lupus Anticoagulant [LA] can prolong phospholipid-dependent coagulation tests e.g. the APTT, giving the impression of a potential bleeding disorder BUT
2.
In vivo Antiphospholipid antibodies may promote thrombosis (Antiphospholipid syndrome [APS]) but in some individuals the presence of the antibody may be entirely asymptomatic and they may occur after, for example, infection.
It is important to identify APLs because they may explain thrombotic episodes and recurrent first trimester miscarriage. In addition if not recognised, a LA can prolong an APTT and subsequent factor assays may be misinterpreted as indicating a coagulation factor deficiency.
A Lupus Anticoagulant can on occasion lead to a bleeding
disorder. This is rare and arises either because of thrombocytopaenia or alternatively because of acquired Prothrombin [Factor II] deficiency.
The diagnosis of the Antiphospholipid Syndrome [APS] requires a combination of at least one specific laboratory test and one or more clinical symptoms - see below:
| Clinical Criteria | |
|---|---|
| Vascular thrombosis | a. One or more clinical episodes of arterial, venous, or small vessel thrombosis, in any tissue or organ. Thrombosis must be confirmed by objective validated criteria i.e. unequivocal findings of appropriate imaging studies or histopathology. b. Patients <50 years of age with an unprovoked venous thromboembolism [VTE]; ischaemic stroke, TIA or other evidence of brain ischaemia c. VTE at an unusual site d. Recurrent VTE with no clear explanation |
| Pregnancy morbidity | a. One or more unexplained deaths of a morphologically normal fetus at or beyond the 10th week of gestation b. One or more premature births of a morphologically normal neonate before the 34th week of gestation because of: (i) eclampsia or severe pre-eclampsia or (ii) recognized features of placental insufficiency c. HELLP syndrome d. Recurrent first trimester miscarriages with maternal anatomic or hormonal abnormalities and paternal and maternal chromosomal causes excluded |
| SLE | Screening for a LA is part of the diagnostic evaluation of a patient with suspected SLE. |
| Consider screening in: | a. ITP b. Livedo reticularis c. Patients <50 years of age with non-criteria clinical manifestations d. Patients <50 years of age when the provoking event is disproportionally mild e. An unexplained prolongation of the APTT |
| Laboratory Criteria At least 2 positive tests for antiphospholipid antibody 12 weeks apart |
|
|---|---|
| Directly | ELISA (enzyme-linked immunosorbent assay) Principles: The three characteristics of relevance for antiphospholipid antibodies are the target antigen, the isotype and the titre. To be significant the antiphospholipid antibodies must be: a) Directed against either cardiolipin (aCL) or β2-glycoprotein-I (anti-β2GPI) b) IgG and/or IgM c) Present in medium-high titre (i.e. >40 GPLU [IgG] or MPLU [IgM] for aCL or >99th percentile for either aCL or anti-β2GPI. Cardiolipin is found almost exclusively in the inner mitochondrial membrane where it performs an essential role in regulating the enzymes involved in mitochondrial energy metabolism. The term 'cardiolipin' originates from the fact that it was first isolated from bovine heart in the early 1940s and formed the basis of the Wasserman test for syphilis. It was originally thought that APLs were autoantibodies directed against anionic phospholipids and which disrupted the assembly of the Tenase and Prothrombinase complexes. However, it was subsequently shown that these were antibodies directed against phospholipid-binding proteins - β2GPI and occasionally Prothrombin. β2-glycoprotein I [β2GPI] - also known as Apolipoprotein H - is a multifunction protein which, in addition to binding to cardiolipin and inducing functionally relevant conformational change, also interferes with platelet aggregation by inhibiting serotonin release and interferes with various steps in the coagulation pathway. β2GPI has five domains and multiple studies have shown that antibodies to the N-terminal domain [Domain I]) are most closely linked to development of thrombosis. The subset of antibodies that bind β2GPI correlate strongly with the thrombotic complications of APS. |
| Indirectly | Through their effect on phospholipid-dependent coagulation assays Principles: Antiphospholipid antibodies can affect the phospholipid used in some laboratory tests of coagulation (e.g. the APTT) and produce a prolonged clotting time. This effect may be overcome by adding sufficient excess of phospholipid that the antibody is overwhelmed [neutralised] and the in vitro clotting time shortens. Demonstration of the presence of an antiphospholipid antibody by coagulation tests requires: a) Prolongation of a phospholipid dependent coagulation test AND b) Correction of that prolongation by adding an excess of phospholipid or otherwise eliminating the effect of any APL OR c) comparison to a phospholipid independent confirmatory test. The tests used for this purpose include: a) Dilute Russell Viper venom test (DRVVT) b) Silica clotting time (SCT) c) Kaolin clotting time (KCT) d) The Textarin/Ecarin time e) Taipan venom time (TVT) f) Factor V ratio No one test will detect all Lupus Anticoagulants and for any given test detection may vary between manufacturers. At least two different tests should therefore be used. |
The diagram below shows a flowchart for the investigation of a case of suspected APS:
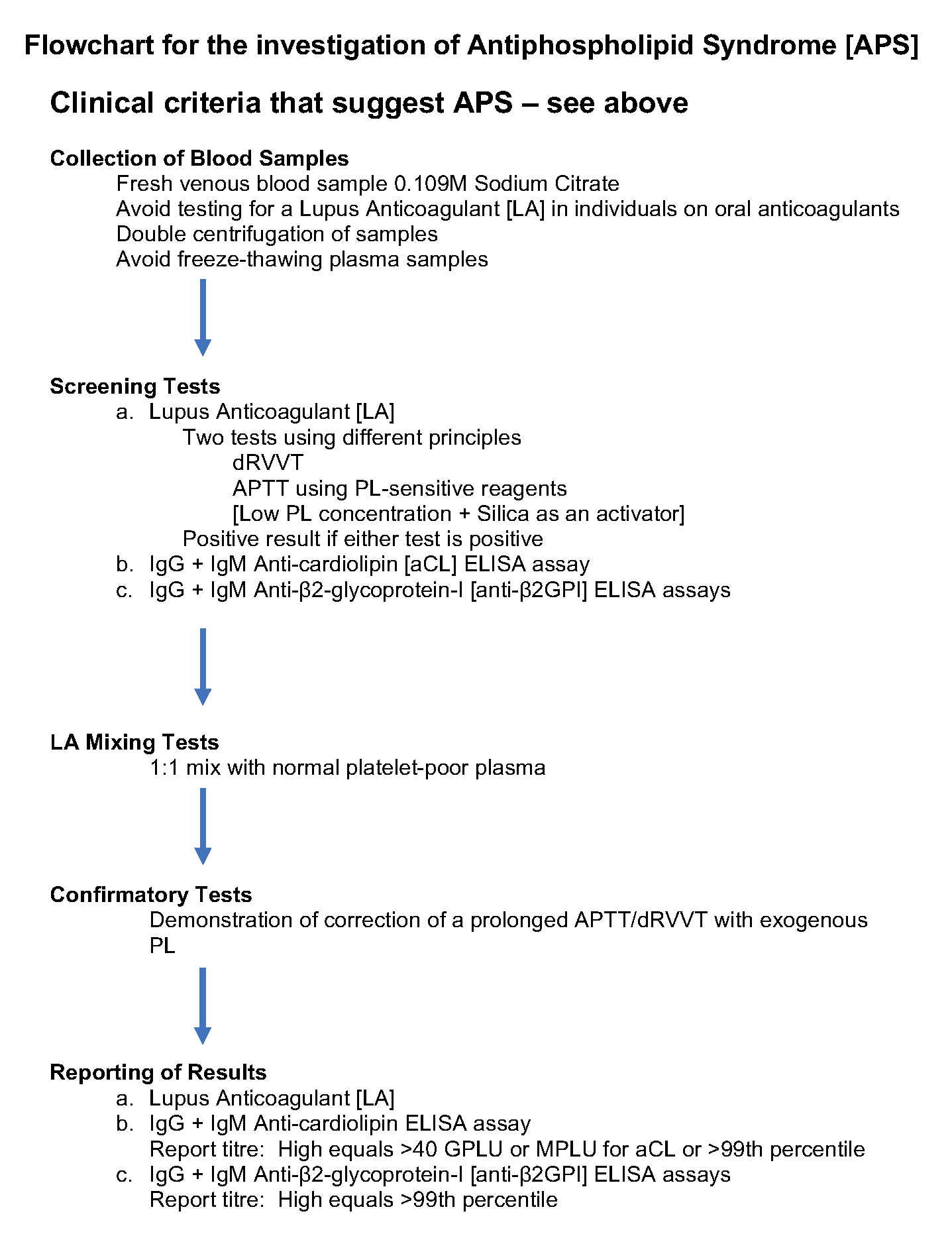
When screening for a Lupus Anticoagulant, two tests based on different principals should be used. Currently the ISTH SSC working party on antiphospholipid antibodies recommends the Silica Clotting Time [SCT] and the dilute Russell Viper Venom Time [dRVVT]. Ellagic acid may show acceptable sensitivity but it is important that laboratories evaluate the sensitivity of their reagents to characterised LA positive samples.
Mixing Studies: The ISTH have advised two methodologies for the interpretation of mixing studies when screening for a LA:
1. Mixing-test specific Reference Interval. Historically laboratories have used the mean + 2.0 Standard Deviations [SD] [97.5th centile for normally distributed data] as a cut-off. The ISTH [2009] recommended the 99th centile [mean +2.3 SD for normally distributed data] which would improve specificity but reduce sensitivity.
If the clotting time of a 1:1 mixture is >99th percentile [or >97.5th centile if using this as a cut-off] of the
distribution of the clotting times recorded for plasma
samples from healthy donors, a confirmatory assay
for a LA should be performed i.e. the SCT or dRVVT with high PL concentration to demonstrate the PL-dependence of the antibody.
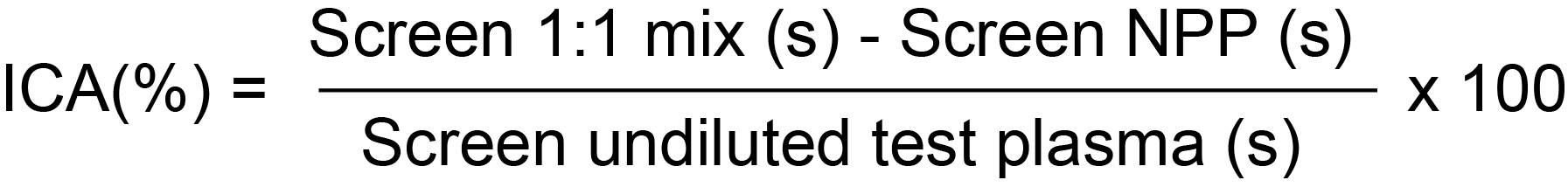
2. Index of Circulating Anticoagulant [ICA]:
Mixing tests introduce a dilution factor and may lead to a false negative LA result. Samples that generate a negative result on mixing but have a prolonged APTT-based test and/or dRVVT
and a positive confirmatory tests should be considered positive for the presence of a LA. Alternative mix ratios e.g. 4:1 patient plasma:normal pooled plasma may be used if validated by the laboratory.
What Test Next?
To complete testing for antiphospholipid antibody, patient samples should be tested for antiphospholipid antibodies twice and at an interval of 12 weeks.
A full blood count [FBC] should also be checked since antiphospholipid antibodies may cause an immune thrombocytopaenia. Antiphospholipid antibodies can also cause acquired Prothrombin deficiency and in patients with APL and a history of bleeding it is of value to measure Prothrombin [Factor II] levels.
Assigning aPL Profiles
Assigning a risk profile is important as it has both diagnostic and therapeutic implications. The presence of a LA is generally considered to confer a high risk of thrombotic events. In addition triple positivity i.e. a Positive LA, high titre aCL and anti-β2GPI antibodies - appears to confer a high risk of thrombosis. A number of studies have shown that antibodies to the N-terminal domain of β2GPI [Domain I] are closely linked to development of thrombosis. See Comments and References.
Click HERE to return to the top of the page.
